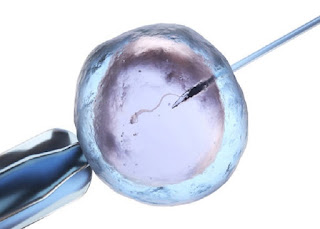
Fresh vs. Frozen Embryo Transfer: Exploring the Differences
There are many decisions to make on your journey to becoming
a parent. Which infertility clinic is a good fit? What treatments are you
willing to undergo? Is it better to transfer fresh or frozen embryos for IVF
(In Vitro Fertilization)? Luckily, your treatment team can help guide you to
the choices that are right for you, and Dr. Walid Saleh of SIRM Dallas in
Dallas, Texas can give you some insight into the pros and cons of fresh versus
frozen embryo transfer below.
A Fresh Perspective
All embryos start out fresh. In a woman’s initial IVF cycle,
she takes medication to first “quiet” the ovaries followed by medication to
stimulate them to produce extra eggs. After the eggs have been surgically
retrieved, they are fertilized. The resulting embryos grow in a special
incubator until they are ready to be transferred to the uterus. In most cases,
one embryo is selected for transfer and the remaining embryos are frozen. Fresh
cycles were, for decades, the gold standard…until the last few years when rapid
advancements in freezing and cryopreservation methods improved the outcome of
frozen embryo transfers.
Back in the Day
First, a little history on frozen embryo transfer (FET).
Embryos were initially frozen slowly which caused intracellular ice to form;
unfortunately, the ice often damaged the embryos. Many damaged embryos didn’t
survive, and those that did had very low potential for successful implantation.
However, in the last several years we’ve seen a dramatic increase in the
quality of frozen embryos due to the introduction of vitrification.
Vitrification is an ultra-rapid freezing method that freezes the embryo
approximately 60,000 times faster than the older method of freezing. This
process takes ice formation out of the equation, resulting in a significant increase
in viable embryos with successful implantation and pregnancy potential equal to
fresh embryos.
If you think frozen embryo transfers may be right for
you, schedule an
appointment at SIRM Dallas in Dallas, Texas to learn more.
Timing is Everything
Another reason we see markedly higher FET success rates now
than several years ago is that the timing of when the embryo is frozen has
changed. It’s been shown that freezing blastocysts (embryo at day 5-6) has a
better outcome than freezing early-cleaved embryos (day 2-3). In many cases
embryos that don’t successfully develop to the expanded blastocyst stage are
aneuploid (chromosomally compromised) and don’t result in healthy babies. An
additional benefit of frozen embryo transfers using expanded blastocysts is
that fewer embryos – because we’re able to determine which are most viable –
need to be transferred. This means we can minimize the chance of a multiple
pregnancy, along with the inherent risks to both mom and baby.
Fresh or Frozen?
At this point, studies show that successful outcomes using
frozen embryo transfers are about equal to those of fresh embryo transfers. The
slight edge that fresh embryo transfer may have is that, typically, the best
embryo is selected for the first transfer. However, there are some key benefits
that make FET appealing:
Because you underwent ovarian stimulation and egg retrieval
for your fresh cycle, you won’t have to go through it again. The medications
necessary to prepare your body for FET have fewer potential side effects and
take less of a toll on your body.
Many patients report that FET cycles are not nearly as
stressful as fresh cycles since they already know they have viable embryos.
It’s easier to schedule and plan for FET cycles than fresh
cycles.
If you’d like to learn more about how fresh and/or frozen
embryo transfers and IVF may benefit you, schedule an
appointment at SIRM Dallas in Dallas, Texas to meet with Dr.
Saleh and discuss your options.



Comments
Post a Comment